The Silent Whispers: Breast Cancer Early Detection & Symptoms in 2026

The Global Crisis: 2026 Statistics
Breast cancer remains the most diagnosed cancer worldwide. As we step deeper into 2026, the numbers tell a compelling story:
- Prevalence: Over 2.3 million new cases are diagnosed annually globally.
- Survival: The 5-year survival rate for localized breast cancer is now 99%. This is a testament to early detection.
- Younger Demographics: There is a slight, unexplained rise in diagnoses among women under 40. This makes "knowing your normal" critical even for younger women.
Early detection is not just a medical recommendation; it is a life-saving protocol. When caught in Stage 0 or 1, treatments are less invasive, and survival is nearly guaranteed.
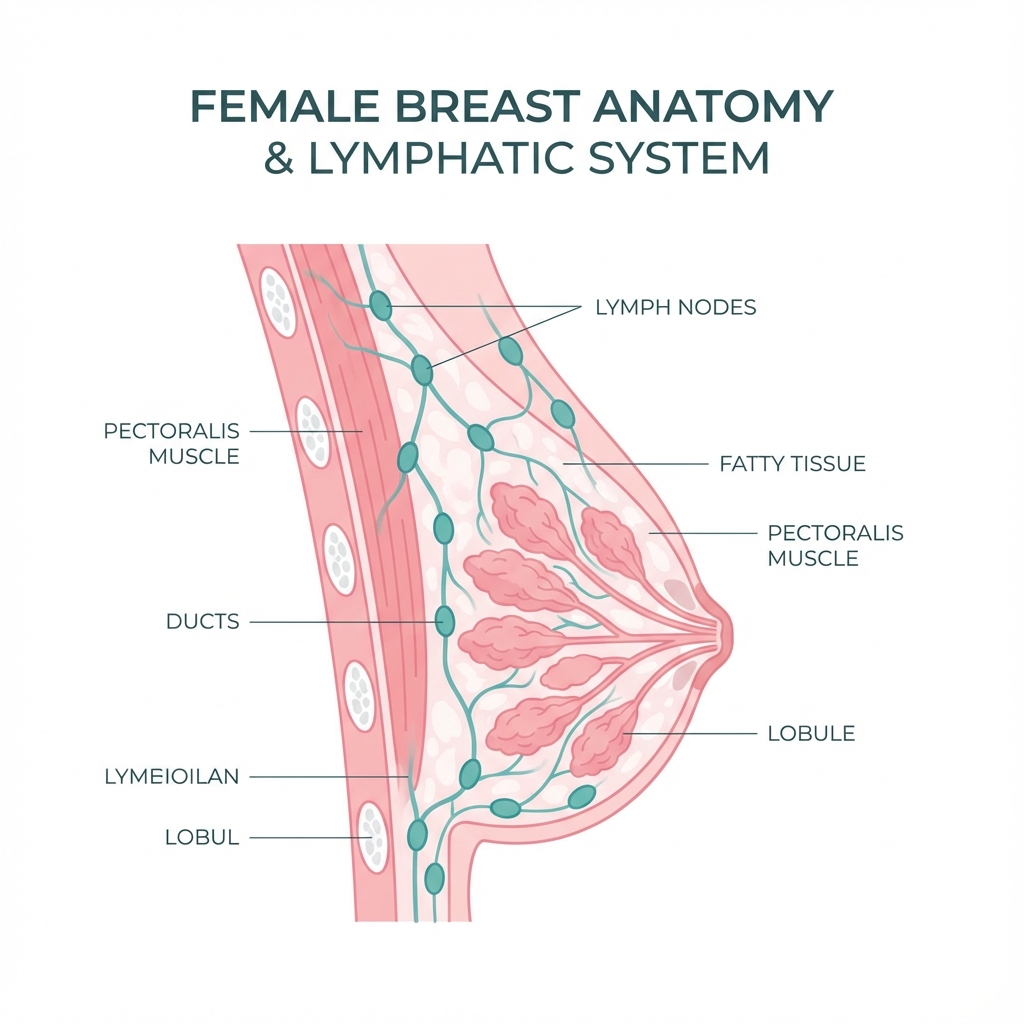
Part 1: Anatomy 101 – Know Your Terrain
To understand cancer, you must first understand the landscape of the breast. It is a complex organ designed for function, but its cellular activity makes it vulnerable.
The Structures
- Lobules: These are the milk-producing glands. Cancer starting here is called Lobular Carcinoma. It is often sneakier and harder to detect on mammograms because it grows in sheets rather than lumps.
- Ducts: The thin tubes that carry milk from the lobules to the nipple. 70-80% of all breast cancers start here (Ductal Carcinoma).
- Stroma: The fatty and connective tissue that surrounds the ducts and lobules.
- Lymph Nodes: The bean-shaped filters clustered in your underarm (axilla) and collarbone. This is the "interstate highway" cancer uses to spread to the rest of the body. Checking your armpits is just as important as checking your breasts.
Part 2: The Symptoms (It's Not Just a Lump)
While a palpable lump is the most classic sign, relying solely on it can be dangerous. Many aggressive cancers, like Inflammatory Breast Cancer, present without a distinct mass.
The "Hidden" Signs
- Dimpling (Peau d'orange): If the skin on your breast starts to look like the peel of an orange (thickened and pitted), this is a red flag. It indicates that cancer cells are blocking the lymph vessels in the skin.
- Nipple Changes:
- Retraction: A nipple that suddenly turns inward (inverted) when it used to point out.
- Direction: A nipple that points in a different direction than usual.
- Crusting: Flaky, red, or crusty skin on the nipple (Paget's Disease of the Breast).
- Discharge: Spontaneous fluid coming from the nipple without squeezing. Bloody, brown, or clear fluid is concerning. Milky discharge (galactorrhea) is usually hormonal but should still be checked.
- Heat & Redness: A breast that feels hot to the touch, looks red/purple, or feels heavy/swollen. This can be mistaken for mastitis but can be a sign of Inflammatory Breast Cancer.
- Swollen Lymph Nodes: sometimes the first sign of breast cancer is a lump in the armpit (axilla) or above the collarbone, even if the breast feels normal.
🚩 Red Flag: The "Painless" Lump
A common myth is that "cancer hurts." In reality, most early-stage cancerous lumps are painless, hard, and immovable (they feel like a rock anchored in the tissue). However, some cancers do cause pain. Rule of thumb: If any change lasts more than 2 weeks, see a doctor. Pain is not a reliable filter.
Part 3: The Risk Factors – What You Can (and Can't) Control
Understanding your risk profile helps you advocate for the right screening plan.
Uncontrollable Factors
- Gender: Being a woman is the #1 risk factor. (Men get it too, but rarely).
- Age: Risk increases as you get older. Most cancers are found in women 55+.
- Genetics: Inherited mutations (BRCA1, BRCA2, PALB2, CHEK2).
- Dense Breast Tissue: Having more glandular tissue than fat makes mammograms harder to read and slightly increases cancer risk itself.
- Menstrual History: Starting periods early (before 12) or menopause late (after 55) exposes you to more lifetime estrogen.
Controllable Lifestyle Factors
- Alcohol: There is a clear link between alcohol intake and breast cancer risk. Even 1 drink a day increases risk slightly.
- Weight: Being overweight after menopause increases risk because fat tissue produces estrogen.
- Physical Activity: Regular exercise lowers estrogen levels and boosts the immune system.
Part 4: The Self-Exam (BSE) – A Monthly Ritual
In 2026, some organizations debate the utility of BSE. We believe that breast awareness is non-negotiable. You can't notice a change if you don't know what "normal" feels like.
The Protocol
Do this 3-5 days after your period starts. This is when your breasts are least hormonal and lumpy. If you are menopausal, pick the same date every month (e.g., the 1st).
- Visual Check:
- Stand in front of a mirror, topless.
- Put hands on hips and press down (this flexes the chest muscles).
- Look for asymmetry across the breasts, changes in shape, or skin dimpling.
- Raise arms overhead and look again.
- The Palpation (Touch):
- Lie down. Place your left hand behind your head.
- Use the pads (not tips) of your three middle fingers on your right hand.
- Use three levels of pressure: Light (skin), Medium (tissue), Deep (rib cage).
- The Pattern: Use a spiral motion starting at the nipple and working outward, OR an up-and-down lawnmower pattern. Cover the entire area from collarbone to bra line, and from armpit to cleavage.
- The Squeeze: Gently squeeze the nipple to check for discharge.
- Repeat on the other side.

Part 5: Screening Technology in 2026
The "Squish" (mammogram) is still the gold standard, but it has upgraded.
1. 3D Mammography (Tomosynthesis)
Traditional mammograms took 2D pictures (like a flat map). 3D mammography takes slices of the breast (like a CT scan). This allows doctors to see "behind" structures.
- Benefit: Reduces false positives by 40%.
- Benefit: Finds 41% more invasive cancers.
- Standard: In 2026, this is the default standard of care.
2. Breast Ultrasound
Used as a supplemental tool, especially for women with dense breasts.
- How it works: Uses sound waves.
- Differentiation: It is excellent at telling the difference between a fluid-filled cyst (benign) and a solid mass (suspicious).
3. Breast MRI
The most sensitive tool available. It reserves for high-risk patients (lifetime risk > 20%).
- Pros: Catch tiny cancers mammograms miss.
- Cons: High rate of false positives (finding things that aren't cancer).
4. AI-Assisted Screening (The 2026 Revolution)
Artificial Intelligence is now routinely used to "second read" mammograms. AI algorithms can detect subtle pixel patterns invisible to the human eye, flagging areas for the radiologist to re-check. This has improved early detection rates significantly.
Part 6: Genetic Testing (BRCA & Beyond)
Knowledge is power, but it can be scary. Genetic testing is recommended if you have a strong family history (multiple relatives with breast/ovarian cancer, male breast cancer, or young diagnoses).
- BRCA1 & BRCA2: The most famous mutations. Risks can be up to 70-80% lifetime risk.
- PALB2: The "Partner and Localizer of BRCA2." Mutations here carry a risk almost as high as BRCA2 (40-60%).
- CHEK2 & ATM: Moderate risk genes (20-30% lifetime risk).
Prophylactic Options
Women with high-risk mutations often face a difficult choice:
- Increased Surveillance: MRI and Mammogram alternating every 6 months.
- Chemoprevention: Taking Tamoxifen to lower risk.
- Prophylactic Mastectomy: Removing breast tissue before cancer develops. This reduces risk by ~95%. It is a deeply personal, brave decision.
Conclusion: Don't Let Fear Win
The fear of finding a lump often stops women from checking. But remember: Finding it early is the best case scenario. A Stage 1 diagnosis is a bump in the road; a Stage 4 diagnosis is a mountain.
Take 10 minutes once a month. Know your body. Trust your gut. If something feels wrong, demand an answer until you are satisfied. You are your own best advocate.



